Not sure whether your pain points to a bulging disc vs herniated disc? You’re not alone. These two spine conditions share overlapping disc injury symptoms, but the cause, imaging findings, and best next steps can…
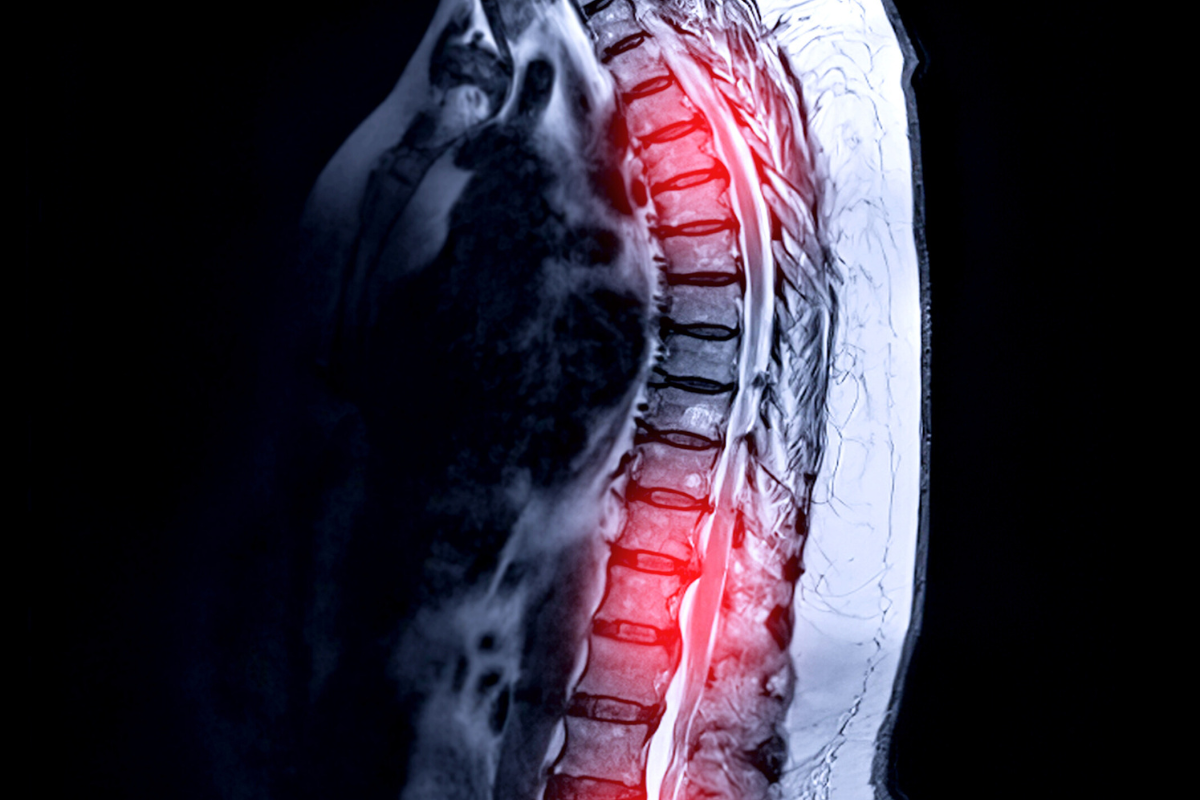
A spinal cord injury (SCI) interrupts the neuronal pathways from the brain to the spinal cord, causing varying degrees of paralysis. A recent investigation sought to identify brain regions that influence walking recovery following incomplete SCI, aiming to enhance this recovery. Researchers developed a comprehensive brain-wide atlas that examined transcriptionally active neurons, particularly those projecting to the spinal cord, and their role in walking recovery after SCI. The analysis highlighted the lateral hypothalamus (LH) as a significant contributor. Experimental evidence indicated that glutamatergic neurons within the LH, specifically LHVglut2, play a crucial role in walking recovery post-SCI. Enhancing the activity of these neurons was shown to facilitate this recovery process.
This discovery led to the implementation of deep brain stimulation targeting the LH (DBSLH) in animal models, including mice and rats with SCI. The stimulation not only improved immediate walking abilities but also instigated longer-lasting recovery outcomes through the reorganization of remaining neuronal pathways from brainstem regions. A preliminary clinical study indicated that DBSLH could significantly enhance walking in two participants with incomplete SCI. Notably, improvements were sustained even after the stimulation was turned off, suggesting a potential for long-term benefits when combined with rehabilitation efforts. Importantly, no serious adverse events were reported in relation to DBSLH.
The findings from this study underscore the promising potential of precisely targeting specific brain regions to bolster the engagement of spinal cord-projecting neurons, thereby advancing functional recovery following spinal cord injuries. The current data indicates a clear need for further clinical trials to assess the complete safety and efficacy profile of DBSLH. Future investigations will also need to evaluate potential impacts on body weight, psychological well-being, hormonal status, and autonomic functions among participants undergoing this treatment.
Research support for this study came from multiple organizations, including ONWARD Medical, the Swiss National Science Foundation, the Canadian Institutes of Health Research, and the European Research Council, among others. A coordinated effort by various contributors led to the comprehensive execution of the study, including animal experiments, computational analyses, anatomical examinations, and rehabilitation procedures.
Innovative methodologies were pivotal in this research, utilizing advanced imaging techniques for neuronal activity assessment and detailed kinematic analysis for gait evaluation. The compilation of a space-time brain atlas served as a foundational tool for advancing understanding of neuronal interactions in the context of walking recovery. Experimental approaches included optogenetic activation and inactivation of specific neuronal populations in the LH, which aided in delineating their functional roles in gait and mobility post-injury.
In the human-centered aspect of the investigations, the clinical trial involved detailed assessments of walking patterns and movements pre- and post-stimulation, highlighting significant gains in mobility attributed to DBSLH. Participants demonstrated improved kinematic scores which positively correlated with the stimulation, indicating an enhanced ability to perform voluntary movements and improved overall locomotion.
As a final note, this research represents a significant stride toward developing targeted therapeutic strategies for individuals facing the challenges associated with spinal cord injuries. The innovative application of deep brain stimulation, combined with ongoing rehabilitation, presents a promising avenue for restoring functional mobility in patients dealing with the long-term effects of SCI. The progress achieved thus far encourages continued exploration and validation of these approaches in larger clinical settings to optimize recovery interventions for individuals affected by these life-altering injuries.