Those who are seeking degenerative disc disease treatments have probably come across facet nerve ablation in their searches. But, is this an effective method of treating your degenerative disc disease symptoms? For many, facet nerve…
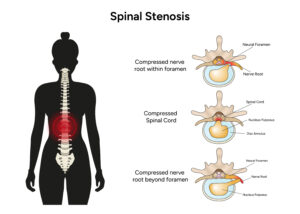
In general terms, spinal stenosis involves the narrowing of the spinal canal. Because the spinal canal houses the spinal cord and nerve roots, these components can easily become compressed. Most of the time, this problem occurs in the neck and the lower back.
Additionally, spinal stenosis is caused by age-related spinal degeneration and wear-and-tear changes related to osteoarthritis. With age, bone spurs, swollen ligaments, and herniated disc material may begin to crowd the spinal canal. In less common cases, some people are born with narrow spinal canals. These people are more prone to developing the condition at a younger age.
There are three basic types of spinal stenosis and they are mainly categorized by the region of the spine that is affected.
Spinal Stenosis Resources
Spinal Stenosis Locations
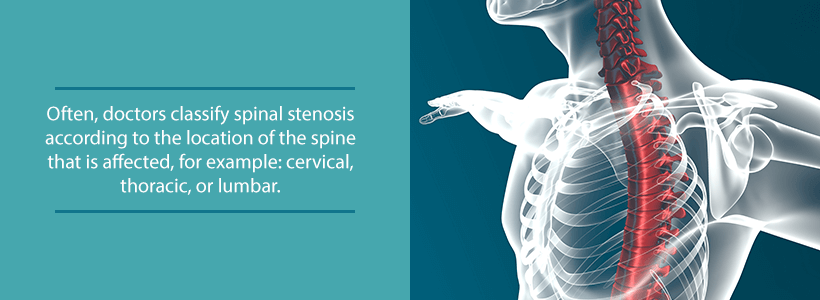
There are two main ways in which doctors categorize spinal stenosis types. The first way breaks down these types by their location:
- Lumbar Spinal Stenosis: Lower back region
- Thoracic Spinal Stenosis: Middle back region
- Cervical Spinal Stenosis: Upper back region
Additionally, doctors may categorize SS types by the part of the spinal column that the condition narrows:
- Foraminal Stenosis: Narrowing occurs in the small openings that allow nerve roots to exit the spinal column
- Lateral Recess Stenosis: Narrowing occurs in the back of the spinal canal where the nerve roots initially branch off
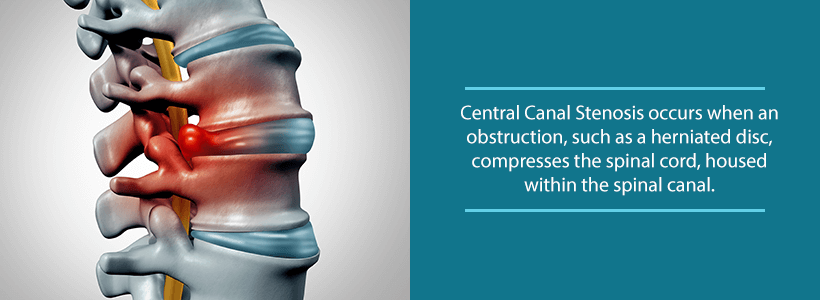
- Central Canal Stenosis: Narrowing occurs in the main spinal canal, which protects the spinal cord
The common thread between these conditions is debilitating symptoms and chronic pain. Sometimes, SS does not cause pain, but it will in cases that result in nerve compression. In these cases, patients should always seek professional treatment.
Foraminal Stenosis
This type of spinal stenosis is the most commonly occurring type. Sometimes, doctors or medical experts may refer to foraminal stenosis as lateral spinal stenosis. In the back of the spine, there are side holes that nerve roots exit through. Experts refer to these anatomical structures as neuro-foramen. In the neuro-foramen, bone spurs that have developed from a degenerating disc or arthritic facet joint can press on these nerve roots. As a result, the narrowing space traps the emerging nerve roots. Speaking visually, this type of spinal stenosis literally pinches the nerves.
Central Canal Stenosis
A membranous sheath of the dura mater known as the thecal sac surrounds the spinal cord. Narrowing of the central canal in the lumbar area leads to compression of this spinal component. This narrowing can cause pressure on the nerve bundle located at the end of the spinal cord (known as the cauda equina). Additionally, this narrowing may also lead to the compression of the individual nerves located within the thecal sac.
Far Lateral Stenosis
In some cases, narrowing occurs beyond the neuro-foramen. Usually, this development stems from bone spurs (which form bulging discs), the facet joints, herniated discs, and ligamentum hypertrophy. When this narrowing occurs to the side of the neuro-foramen, experts call it far lateral stenosis. With spinal stenosis, there is generally a combination of far lateral and foraminal stenosis.
Spinal Stenosis Causes
- Formation of bone spurs
- Inflammation of nearby surrounding soft tissue
- Herniated or bulging discs that put pressure on the spinal canal
- Calcification of the spinal ligaments
- Spinal misalignment caused by vertebrae slipping out of place
- Other issues, such as tumors, diseases, or infections
Spinal structures will naturally degrade over time. While this is the case, chronic pain and other debilitating symptoms will only appear in cases where the nerves are pressured.
Spinal Stenosis Symptoms
Symptoms of spinal stenosis will vary by location and other individual factors, however, there are many blanket symptoms that all types share. Some of the most commonly experienced symptoms of spinal stenosis include:
- Burning sensations
- Loss of fine motor skills
- Limited mobility
- Muscle weakness
- Local and traveling pain
- Numbness and tingling
It is important to note that a person may have evidence of spinal stenosis on an MRI or CT scan but is unaffected in any meaningful way. In such cases, symptoms sometimes gradually appear and worsen with time. Therefore, it is important to recognize the signs of spinal stenosis and seek professional medical care when necessary.
Diagnosis
If you experience neck or back pain that lasts for more than a few days, then you should consider visiting your primary care physician. Additionally, it is not uncommon to experience anxiety involving this process, but this can be alleviated by taking it slow and asking questions. Generally speaking, reaching a diagnosis for most conditions involves three important steps:
- Symptom Discussion & Medical History: In most cases, a diagnosis starts with a question-and-answer session between you and your doctor. Your doctor will ask you to describe the symptoms you are experiencing, as well as a variety of other factors. This may include facts about your lifestyle, your diet, previous treatments, and other pre-existing medical conditions. Additionally, your doctor may ask you questions about your family’s medical history. This is because many conditions that cause back and neck pain are inheritable.
- Physical Examination: To better understand the source of your symptoms, your doctor will apply pressure around your neck and back. Furthermore, they will also test your range of motion and attempt to identify areas of pain to further understand the source of your symptoms. Unfortunately, this process is usually uncomfortable, but it provides your physician with valuable information.
- Medical Imaging: In order for your doctor to make an accurate diagnosis of spinal stenosis, he or she will often resort to medical imaging. Usually, this comes in the form of an MRI or CT scan, which provides an inside view of the spinal column. These imaging tests will show the exact cause of the narrowing, such as herniated disc material or bone spurs.
Conservative Treatments
Once you have received your diagnosis, your doctor will work with you in order to develop a personalized care plan. Generally, many spinal stenosis patients are actually able to return to normal activities without having to resort to surgery. The reason for this is that a range of more conservative treatments usually brings more meaningful relief from symptoms.
Commonly used conservative methods are:
- OTC and prescription pain medication
- Physical therapy
- Massage therapy
- Low-impact exercise
- Hot and cold compresses
- Corticosteroid injections
- Acupuncture
- Chiropractic adjustments
- Intermittent rest
- Stretching
Minimally Invasive Surgery
Minimally invasive spine surgery is a safer and more effective alternative to traditional open-back procedures. There are two main types of minimally invasive spinal procedures: decompression and stabilization. Both types can be used to treat SS, however the best option for you will depend on your individual case.
Decompression Surgery
This type of minimally invasive surgery is primarily used to treat mild and medium cases of spinal stenosis. Most stenosis patients fall within this category. The two most commonly used minimally invasive decompression surgeries for spinal stenosis are laminotomy and foraminotomy. With decompression surgery, the common goal is to remove the diseased portion of the spine. This may be a bone spur, a herniated disc, or some other abnormality that compresses nerve roots.
A surgeon can typically perform the procedure through a small, 1-inch incision. The smaller incision allows for faster recovery time, less scarring, and less damage to surrounding muscles. Once the incision is made, the surgeon removes the infected portion of the spine and the nerve decompresses. Because this procedure is performed as an outpatient procedure, patients usually return home the same day the surgery is done.
Stabilization Surgery
Stabilization surgery is used for more severe cases of spinal stenosis and may be required to treat chronic symptoms and pain. This procedure is performed through a small incision in the back, side, or neck. The access point depends on the location of the patient’s spinal stenosis. In order to access the affected area, the surgeon will carefully move aside the surrounding muscles to avoid unnecessary damage. Once the spine is accessible, the surgeon then removes the affected area, which is usually a vertebrae or disc. Once your doctor has removed the area, an implant takes its place in order to stabilize the spine. Common examples of minimally invasive stabilization surgery include transforaminal lumbar interbody fusion and anterior cervical discectomy fusion.
If you have pain in your neck or back lasting for more than a few days, please contact us at (855) 853-6542 or fill out a form online. At the OLSS, our board-certified orthopedic surgeons understand that the medical needs of each patient are different. We will work tirelessly to ensure that you receive the personalized care plan you need for your case.